Authored by RJ Tesi via RealClearScience,
Alzheimer’s disease (Alzheimer’s) has long been associated with gray matter pathology, specifically extracellular amyloid plaques and neurofibrillary tangles. However, recent neuroimaging studies have highlighted the importance of white matter abnormalities in the development and progression of Alzheimer’s, suggesting that white matter degeneration and demyelination play a crucial role in the disease. Shifting focus to white matter abnormalities could open up new avenues for understanding Alzheimer’s pathology and identifying potential treatment targets.
Understanding White Matter vs. Gray Matter
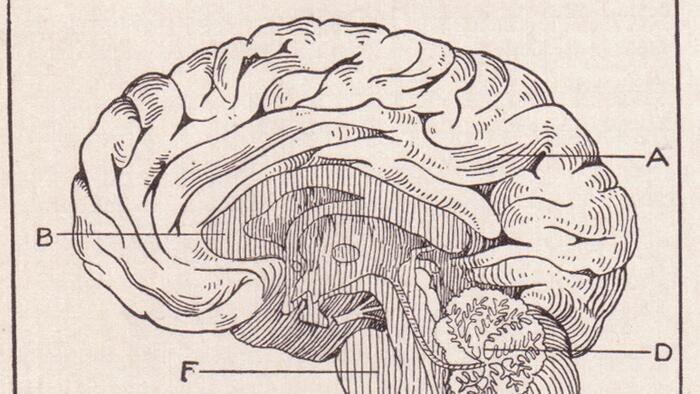
Gray matter consists mainly of neuronal cell bodies where memories are stored and cognitive functions are processed. On the other hand, white matter is composed of myelinated axons that facilitate communication between different parts of the brain and spinal cord. When white matter is diseased, the brain’s ability to function properly is compromised due to the breakdown of myelin and axons.
Evidence Supporting White Matter in Alzheimer’s
While gray matter changes in Alzheimer’s are well-documented, the role of white matter abnormalities in the disease has only recently come to light. Studies have shown that white matter alterations occur early in the disease process and can precede the onset of clinical symptoms. Research has also linked white matter abnormalities to neuropsychiatric symptoms and genetic alterations in myelin proteins, indicating their importance in Alzheimer’s development.
Implications for Alzheimer’s Treatment
Recognizing white matter as a potential therapeutic target opens up new possibilities for treating Alzheimer’s. Addressing white matter disorders could help alleviate the cognitive decline associated with myelin damage. By shifting focus to white matter abnormalities, researchers may be able to develop more effective treatments and potentially work towards finding a cure for Alzheimer’s.
Loading…